Half of the world’s population does not have access to proper healthcare. About 100 million people are driven into poverty because of out-of-pocket health spending each year. Over 930 million people spend at least 10 per cent of their household income on healthcare. These estimates by the World Health Organisation, scary as they are, call for immediate action. We need a universal healthcare system.
Over the last two years, the coronavirus pandemic has brought into sharp focus the imperative need for preventive healthcare in the Indian ecosystem. And if India even works to fulfil the United Nations Sustainable Development Goal 3.8 that advocates “providing universal health coverage for all by 2030”, we will be well on our way towards a healthier nation.
As India traverses the path toward a holistic health policy, the aim should be to facilitate health coverage that includes financial risk protection, access to quality essential healthcare services, and the availability of safe, quality, effective, and affordable essential medicines and vaccines for all.
For families even slightly above the poverty line, the financial implications of hospitalisation are extremely devastating that they can be plunged below the line of poverty post a single hospital visit. Reports suggest that the average hospitalisation cost of Rs 20,000 for an ailment is more than the annual consumer expenditure of nearly half our population. Further, delayed hospitalisation can be crippling and have long-lasting ill effects on a person’s health. The bedrock of a sustainable and effective health system is affordable primary healthcare and can only be achieved by formulating an expansive universal health coverage policy that emphasises as much out-patient care as it does in-patient care.
A Crying Need
Data from the National Family Health Survey–5 (NFHS-5) is encouraging. We have made significant progress on demographic and health indicators such as the total fertility rate (TFR), women‘s education, and child mortality rates, all of which point toward the increased coverage of immunisation, antenatal care (ANC), institutional deliveries, amongst other parameters. And although health indicators have gradually improved, health for all is yet to be achieved.


For families even slightly above the poverty line, the financial implications of hospitalisation are extremely devastating that they can be plunged below the line of poverty post a single hospital visit. Reports suggest that the average hospitalisation cost of Rs 20,000 for an ailment is more than the annual consumer expenditure of nearly half our population. Further, delayed hospitalisation can be crippling and have long-lasting ill effects on a person’s health. The bedrock of a sustainable and effective health system is affordable primary healthcare and can only be achieved by formulating an expansive universal health coverage policy that emphasises as much out-patient care as it does in-patient care.


To capture the advantages of a universal healthcare system at the Central level, a national policy is the need of the hour as it will not only lower healthcare costs for individuals but also for the economy as the end control over the prices of medication and services remains with the government.
The National Health Policy (NHP) 2017 does have provisions for free primary care in public hospitals that provide referrals to hospitals, free drugs, and cheap or free diagnostic and emergency services. However, gaps remain.
Under the Ayushman Bharat scheme, the Government of India aims to secure the lives of 50 crore individuals that comprise 10.74 crore poor families – including both rural and urban areas – with a defined benefit cover of Rs 5 lakh per family. The scheme covers nearly 40 per cent of the population targeting the poorest and the vulnerable. With initiatives like the National Health Protection Scheme and Pradhan Mantri Jan Arogya Yojayan (PM-JAY) already in place, we have set out on the right path, but the journey is long.
Preventive Healthcare in India
Apart from the lack of awareness around common diseases such as Chronic Obstructive Pulmonary Diseases (COPD), diabetes, and hypertension, the overall health expenditure of India also hinders the potential growth of the preventive healthcare system in India.
As per a 2019 report, preventive healthcare accounted for a meagre 11 per cent of India’s overall healthcare expenditure. With the country struck by a loop of lifestyle-oriented diseases, the need for strategising a holistic healthcare plan is at its peak.
Under the Ayushman Bharat scheme, the Government of India aims to secure the lives of 50 crore individuals that comprise 10.74 crore poor families – including both rural and urban areas – with a defined benefit cover of Rs 5 lakh per family. The scheme covers nearly 40 per cent of the population targeting the poorest and the vulnerable. With initiatives like the National Health Protection Scheme and Pradhan Mantri Jan Arogya Yojayan (PM-JAY) already in place, we have set out on the right path, but the journey is long.

Given this scenario, the Enso Group’s idea of launching Enso Healthcare is a step in the right direction toward India’s goal of making healthcare facilities accessible to all. We have also joined hands with Russia-based RDIF for procuring Sputnik V and Sputnik Light vaccines from India and other parts of the world. Sputnik V and Sputnik Light vaccines are double-shot vaccines taken as a preventive solution to COVID-19. Sputnik V is known to have 91.4 per cent efficacy, while Sputnik Light has an efficacy of about 80 per cent.
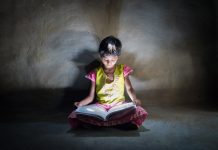
Healthcare for Children
In March 2022, the Centre began vaccinating adolescents in the age group of 12 to 15 years as part of the ongoing preventive measures to fight the pandemic. This assumes added significance as schools across the country begin physical classes.
There is no centralised public data in India on the number of children that needed hospital care due to the coronavirus infection, but authorities in other developed nations such as the US and the UK have recorded a rise in hospitalisation in children from the newer variants – Delta and Omicron. Additionally, child health experts and doctors note that children are vulnerable to catching the COVID-19 disease as it is difficult for them to maintain social distancing and wear masks for long in school.
 A report published by the National Institute of Disaster Management (NIDM) in August 2021 recommended expanding existing health facilities for children in the country. With schools reopening and children going back to school, India needs to strengthen and formulate a holistic plan for its national preventive healthcare policy.
A report published by the National Institute of Disaster Management (NIDM) in August 2021 recommended expanding existing health facilities for children in the country. With schools reopening and children going back to school, India needs to strengthen and formulate a holistic plan for its national preventive healthcare policy.
 The NFHS-5 states that the number of Indian women who are anaemic between 15 and 49 years of age saw a significant jump of 57.2 per cent from the 49.7 per cent reported in NFHS-4. As the country battles rising levels of malnutrition, anaemia among women and stunted and wasted growth in children, some States on the brink of public health risks need urgent policy intervention.
The NFHS-5 states that the number of Indian women who are anaemic between 15 and 49 years of age saw a significant jump of 57.2 per cent from the 49.7 per cent reported in NFHS-4. As the country battles rising levels of malnutrition, anaemia among women and stunted and wasted growth in children, some States on the brink of public health risks need urgent policy intervention.
A forward outlook to create a universal healthcare system can be divided into four parts – regular vaccinations, development of public health infrastructure, eradication of diseases and changing lifestyle habits using educating the future generations.
The Way Forward
A forward outlook to create a universal healthcare system can be divided into four parts – regular vaccinations, development of public health infrastructure, eradication of diseases and changing lifestyle habits using educating the future generations.
India, within two decades, received ‘Polio-free Certification’ from the World Health Organisation on March 27, 2014, with the last polio case reported in Howrah, West Bengal, on January 13, 2011. This success story can be the country’s blueprint for making the healthcare arm stronger with vaccinations.
COVID-19 in 2022 is still a looming threat. Despite the availability of vaccines, their administration seems to have been a major issue the Indian Government has been dealing with due to external forces like the circulation of fake jabs and vaccine hesitancy. It is sad to see politics hampering vaccination as this has a direct correlation to strengthening preventive healthcare in the country.
Vaccines in India, especially booster doses, should be allowed to be given by general practitioners via the Aarogya Setu app.
To bolster this process, there should be special emphasis on the development of public health infrastructure such as district hospitals that require renovation and expansion to accommodate India’s growing population in times of need. For this, hospitals should be provided with better supplies and technology-driven high-quality medical equipment.


Akin to the National Disaster Management Authority, a wing should be created under the Health Ministry to facilitate a swift and immediate response mechanism to any health crisis so that the country is better prepared for sudden pandemics such as the coronavirus and ensure that the healthcare system does not collapse. This could also be a global achievement for India to create a pathway for other nations to focus on and add on.
 Among the diseases that circle back to lifestyle changes and habits, smoking, alcohol and drugs have wreaked havoc in society, and it is the collective responsibility of the citizens of this country to make sure future generations breathe healthily.
Among the diseases that circle back to lifestyle changes and habits, smoking, alcohol and drugs have wreaked havoc in society, and it is the collective responsibility of the citizens of this country to make sure future generations breathe healthily.
Further, promoting consciousness of health and healthy habits through sports, sex education and maintaining cleanliness should set the groundwork for formulating an effective, efficient and quality universal healthcare system in India.